Today’s case 12 – Successful selective thoracic duct embolization(TDE)
Today, I will discuss the technique of thoracic duct embolization, which is used to treat chyle leakage resulting from surgical procedures or trauma to the thoracic duct.
Lymphatic intervention to treat chyle leakage is a well-known technique among interventional radiologists, but it is not widely performed.
This is because the technique is relatively complex compared to other vascular procedures, and additionally, the referring physicians may not be aware that chyle leakage symptoms can be effectively treated through this method.
Symptoms caused by chyle leakage, such as lymphedema, chylothorax, mesenteric chylous cyst, and chyluria, can be so debilitating that they significantly reduce the patient’s quality of life over time.

(Img from : https://lymphedemateam.com/lymphedema-vs-lipedema/)
The availability of non-surgical intervention as a treatment option for lymphatic leakage disorders is indeed welcome news for patients suffering from these conditions.
However, as previously mentioned, it’s disappointing that the procedure is not yet widely practiced and is only performed at a select few institutions.
Let’s now begin with the case presentation.
Our patient is a 33-year-old woman.
She was referred to us for chylothorax that developed after a robot-assisted total thyroidectomy, which was performed to treat papillary thyroid carcinoma.
The surgery was conducted at another institution, and she was sent to us because there were no physicians there who could perform the lymphatic intervention.
Her symptoms were concerning; her neck was swollen as if she had severe hypothyroidism. Daily aspiration from the swollen neck, which proved to be ineffective, was conducted, yet the symptoms persisted.
Subsequently, she was referred to our department.
We performed lymphangiography to embolize the thoracic duct, and I was involved in this procedure as the first assistant.
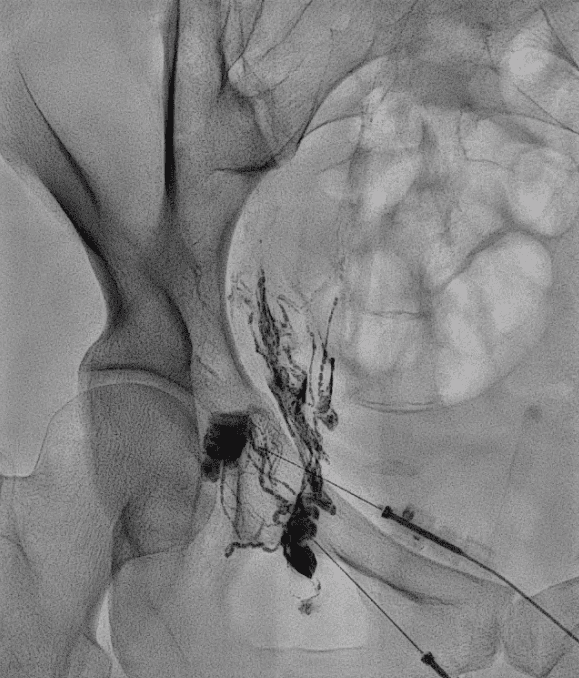
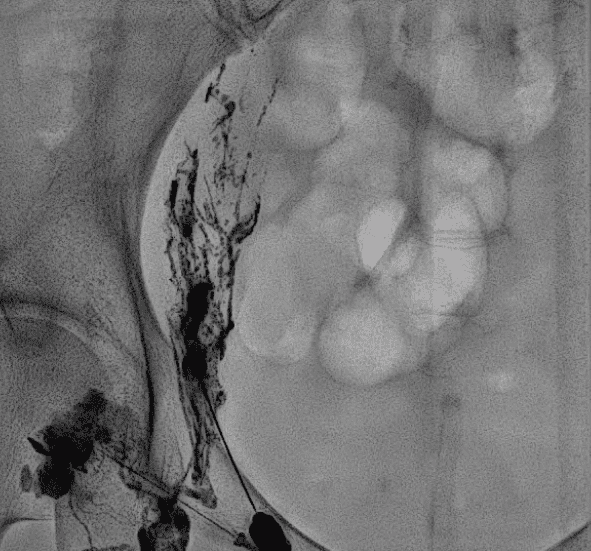



This step is crucial in performing lymphatic interventions and can also be time-consuming if puncturing the thoracic duct is not achieved promptly.










You can see the loop of the micro-guidewire, indicating that it was inside the cavity.



After the procedure, the patient began to eat again.
With the resumption of eating, no additional chyle leakage occurred.
After confirming that eating did not cause a recurrence of the symptoms, the patient was discharged